Introduction:In R/R DLBCL patients receiving CAR T-cell therapy (CAR-T), bridging therapy (BT) with chemotherapy, targeted therapy, and/or radiation therapy (RT) is often administered during the manufacturing window after collection and prior to CAR-T infusion to aid in tumor debulking and/or control symptomatic disease. However, little is known about the optimal type of BT and specifically, the impact BT may have on patterns of failure. Thus, we sought to compare the patterns of failure in patients who received CAR-T for R/R NHL at a single-institution based on the type of BT received. We hypothesize that bridging RT decreases the risk of local recurrence in sites treated with RT prior to CAR-T therapy.
Methods: An IRB-approved single-institution retrospective review was performed of all R/R DLBCL patients who underwent leukapheresis for planned CAR-T with axicabtagene ciloleucel (axi-cel). 20 patients were identified, of whom 1 died before CAR-T infusion and 3 died before day +30 post-CAR-T (D+30) PET/CT scans due to CAR-T related toxicities (n=2) or disease progression (n=1). Of the 16 patients who had D+30 PET/CT scans, demographic, disease, and treatment characteristics, as well as toxicity and survival outcomes, were collected and analyzed. PET/CT scans immediately before CAR-T, as well as D+30, D+90, 6 months, and 1-year post-CAR-T infusion were analyzed, with response assessment per the Lugano classification. FDG-avid (Lugano 4 or 5) lesions on pre-CAR-T scan were recorded as index lesions and compared to residual or new FDG-avid lesions on all available post-CAR-T scans.
Results: Of the 16 patients who had D+30 PET/CT scans, 4 received no BT, 6 received bridging chemotherapy, 5 received bridging RT (median 30 Gy in 10 fxs), and 1 received a Bruton's tyrosine-kinase inhibitor (BTKi) on a clinical trial. At last follow up, 11/15 (73%) were alive (3/4 with no BT, 3/5 with bridging chemotherapy, 4/5 with RT, 1/1 with BTKi) and 8/15 (53%) were without disease progression (3/4 with no BT, 3/5 with chemotherapy, 2/5 with RT, 0/1 with BTKi); one patient was lost to follow up.
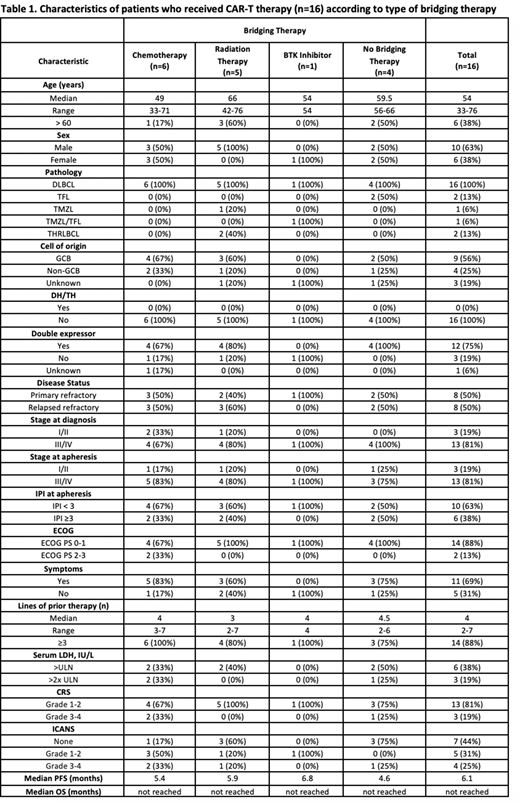
Grade 3-4 cytokine release syndrome (CRS) occurred in 1/4 (25%) patients without BT, 2/6 (33%) patients with bridging chemotherapy, and 0/5 (0%) patients with bridging RT. Grade 3-4 immune effector cell-associated neurotoxicity syndrome (ICANS) occurred in 1/4 (25%) patients without BT, 2/6 (33%) patients treated with bridging chemotherapy, and 1/5 (20%) patients treated with bridging RT. Complete patient, disease, and treatment characteristics, as well as outcomes and toxicities, are summarized in Table 1.
6/16 (38%) patients had metabolic complete response (CR) at D+30 and 6/13 (46%) at D+90. In comparison among type of BT received, D+30 and D+90 CR rates, respectively, were 1/4 (25%) and 2/3 (67%) for no BT, 4/6 (67%) and 3/5 (60%) for bridging chemo, and 1/5 (20%) and 1/4 (25%) for bridging RT.
In analysis of patterns of failure, there were 48 total index lesions identified on pre-CAR-T PET/CT scans. Of those, 20 received no BT, 15 were treated with bridging chemotherapy, 7 with bridging RT, 6 with bridging BTKi. On D+30 PET/CT, the rates of CR were 16/20 (80%) in lesions without BT, 8/15 (53%) in lesions treated with bridging chemo, 6/7 (86%) in lesions with bridging RT. By D+90, the rates of CR were 7/9 (78%) in lesions without BT, 8/11 (73%) in lesions treated with bridging chemo, and 3/3 (100%) of lesions treated with bridging RT. Of the 50 lesions noted on D+30 PET/CTs, 18 (36%) were index lesions on pre-CAR-T PET/CT, and only 4/28 (14%) lesions on D+90 PET/CT were initial index lesions.
Conclusions: Patients who require BT before CAR-T have higher relapse rates, likely reflecting more aggressive disease biology. Bridging RT to CAR-T appears to be safe and effective in providing local control, even at palliative doses, but may not impact overall outcomes. Due to small sample size and retrospective biases, comparison among bridging treatments is limited, and the optimal bridging strategy remains unknown. However, these data suggest that bridging RT should be considered in sites where local control is a priority, such as symptomatic sites or sites where recurrence may cause significant morbidity. Radiating all sites of active disease pre-CAR-T may not improve outcomes though as the predominant pattern of failure appears to be distant. The optimal timing and combination strategies with RT and CAR-T for R/R DLBCL needs to be explored prospectively.
Awan:MEI Pharma:Consultancy;Karyopharm:Consultancy;Genentech:Consultancy;Astrazeneca:Consultancy;Abbvie:Consultancy;Janssen:Consultancy;Pharmacyclics:Consultancy;Sunesis:Consultancy;Gilead Sciences:Consultancy;Kite Pharma:Consultancy;Dava Oncology:Consultancy;Celgene:Consultancy;Blueprint medicines:Consultancy.Desai:Boston Scientific:Consultancy, Other: Trial Finding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal